
Some surgeons regard cases with late diagnosis or missed diagnosis as an absolute contraindication to fasciotomy based on a perceived increased risk of postoperative infection. Patients with late established acute compartment syndrome are not likely to have any functional benefit from fasciotomy. (See "Acute compartment syndrome of the extremities".). As an example, for a patient with a systemic blood pressure of 100/70 mmHg, a compartment pressure exceeding 40 mmHg is indicative of an established acute compartment syndrome. A compartment less than 30 mmHg below diastolic blood pressure is an indication for fasciotomy.

Using the diastolic blood pressure as a reference point for compartment pressures may provide increased diagnostic accuracy for the diagnosis of established acute compartment syndrome.

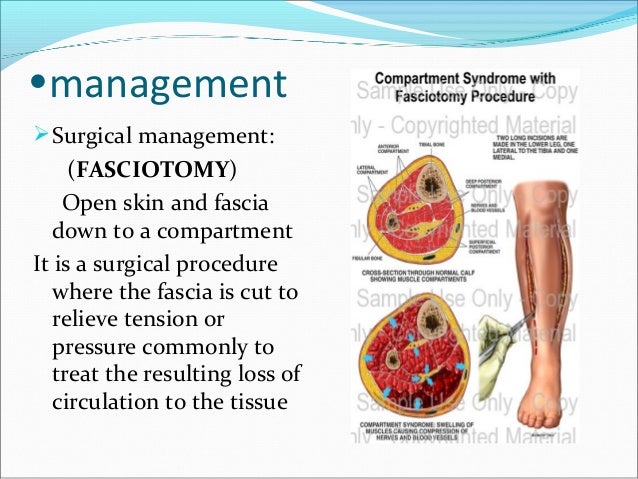
The clinical evaluation and diagnostic criteria for acute compartment syndrome and chronic exertional compartment syndrome are discussed in separate reviews. (See "Patient management following extremity fasciotomy".) Patient management following fasciotomy, including wound care, is discussed elsewhere. Alternative techniques for chronic compartment syndromes are briefly discussed. The indications for and techniques of lower extremity fasciotomy for emergent fasciotomy of the leg, thigh, buttock, and foot will be reviewed here. In addition, patients who suffer from chronic compartment lower extremity syndromes may also benefit from fasciotomy.įor acute compartment syndrome, failure to recognize and decompress the muscular compartments in a timely fashion can compromise the extremity or the patient's life. Although less common, acute compartment syndrome can occur in the thigh, buttock, and foot. The leg is the most frequently affected site in the lower extremity requiring fasciotomy. Once you take up running again, for instance, those familiar symptoms usually come back.INTRODUCTION - Extremity fasciotomy is the only recognized treatment for acute compartment syndrome. Taking a complete break from exercise or performing only low-impact activity might relieve your symptoms, but relief is usually only temporary. Over time, recovery time after exercise may increase.Becomes less intense or stops completely within 15 minutes of stopping the activity.Begins consistently after a certain time, distance or intensity of exertion after you start exercising the affected limb.Pain caused by chronic exertional compartment syndrome typically follows this pattern: Occasionally, swelling or bulging as a result of a muscle hernia.Foot drop, in severe cases, if legs are affected.Numbness or tingling in the affected limb.
Aching, burning or cramping pain in a compartment of the affected limb.Chronic exertional compartment syndrome often occurs in the same compartment of an affected limb on both sides of the body, usually the lower leg. Your lower leg, for example, has four compartments. Your limbs have specific areas of muscle (compartments).


 0 kommentar(er)
0 kommentar(er)
